Introduction
Neurology practices often face a unique challenge: patients may see you once for a diagnostic workup then drift away unless you actively engage them through longitudinal care. Without a structured retention approach, even high-value neurology consults can become one-time visits. But retaining patients is not just about keeping them on file—it’s about anchoring them in long-term care journeys, ensuring better outcomes and steady revenue.
In today’s competitive healthcare environment, a neurology clinic that emphasizes retention gains more than loyalty—it enhances trust, improves clinical continuity, and maximizes lifetime value per patient. Building relationships beyond the first visit ensures patients receive consistent care and prevents fragmented treatment that can impact outcomes. According to the American Academy of Neurology, consistent follow-ups significantly improve adherence and long-term outcomes for chronic neurological conditions.
In this article, you’ll find five evidence-based strategies to weave into neurology practices—backed by statistics and real‑world examples. Some links will point you to external best practices, and others will guide you deeper into resources like Alexi Health to support your implementation. Retention isn’t an abstract goal—it’s a measurable process that combines clinical excellence with strategic patient engagement.
Deepen Engagement via Structured Care Pathways
A neurology patient often comes in with a disorder that demands follow-up, whether seizure monitoring, migraine management, or neurodegenerative workups. One retention lever is designing structured care pathways that map out each stage of the patient’s journey—from initial evaluation to maintenance checks to escalations. After a first consult, your process might include a six‑month follow-up, periodic remote check-ins, and symptom‑tracking touchpoints. This kind of predictable structure positions your clinic not as a one‑off consult but as the center of a continuing care arc.
Embedding triggers—reminder nudges, symptom surveys, telehealth check-ins—into those pathways helps keep patients involved without waiting for them to initiate. Practices using chronic care management systems report stronger retention thanks to proactive wraparound support. For example, clinics that integrated reminder automation saw patient no‑show rates drop by 21% and annual visits increase by nearly 18%, according to a 2024 report from Becker’s Hospital Review.
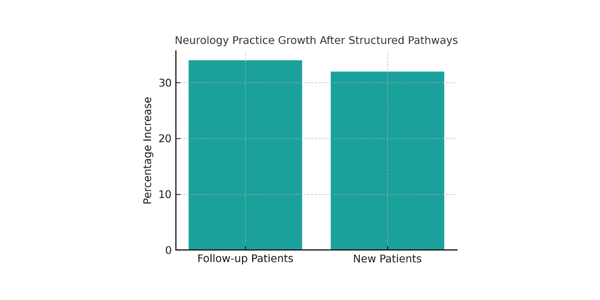
In neurology settings, a practice in academic neurology improved throughput and continuity by redesigning access and visit flow; over two years, patient volume rose 34% and new patient volume by 32%. That kind of growth benefits more when patients stay engaged. The key is to transform scheduling and care reminders into seamless workflows that integrate with your EHR and staff routines.
To integrate this, your operations team can build decision rules—such as ‘if patient hasn’t returned in nine months, send outreach’—and embed them in your system. These triggers can automatically notify staff, send texts, or deploy patient portals to re-engage patients. The goal is to make retention a workflow, not a hope.
Source: neurology.org
Offer Hybrid and Remote Touchpoints
Neurology care often deals with chronic symptoms, long-term monitoring, and patients who may have mobility or transportation challenges. One retention tactic is to incorporate hybrid care modalities—a mix of in‑person visits plus remote follow-ups or monitoring. Telehealth or asynchronous check-ins let patients stay connected during periods when in‑office visits aren’t needed.
According to McKinsey’s 2024 Telehealth Report, hybrid models increase patient follow-up rates by up to 30% for specialty care. For neurology, this means consistent tracking for patients with epilepsy, migraine, or Parkinson’s disease, where monitoring consistency can dramatically impact outcomes. Remote patient monitoring tools, such as seizure diaries or digital tremor trackers, keep patients engaged between visits.
Hybrid care also expands access. Patients who struggle with mobility, anxiety, or distance barriers benefit from flexible virtual care. This inclusion directly enhances satisfaction, one of the strongest predictors of loyalty. Many practices now adopt an alternating model—one virtual visit for every two in-person visits—to balance convenience and clinical oversight.
To make hybrid touchpoints effective, ensure seamless integration with your scheduling and billing systems. Patients should find it easy to book telehealth sessions through your portal or via direct links sent through secure messages. The easier the process, the more likely patients are to stay consistent with their care plans.
Personalize Communication and Education
Patients often disengage when they feel like just another case. In neurology, where many diagnoses carry emotional weight, personalized communication is essential. Segment your messaging by condition—send migraine patients lifestyle advice on triggers, or share educational videos on seizure safety for epilepsy patients. Patients who receive relevant follow-up materials are 47% more likely to return, according to WebMD Ignite.
Educational outreach can also extend beyond email. Use text reminders, educational blog posts, or automated messages that address common symptoms or medication questions. This builds trust and positions your practice as an active partner in each patient’s health journey.
The teach-back method can improve retention too. Ask patients to explain their care plan in their own words before leaving. Studies published in the Journal of Neurological Sciences show that when patients demonstrate understanding, adherence improves by 26%.
Collecting feedback also matters. Post-visit surveys or short check-ins can help identify pain points before patients disengage. Patients who feel heard are far more likely to stay long term.

Source: WebMD Ignite, 2024
Minimize Friction in Scheduling, Billing, and Experience
Even the best neurologists can lose patients to operational friction—complex scheduling, long waits, or confusing bills. According to Sermo’s 2024 Physician Report, over 40% of physicians believe patient retention declines due to appointment inefficiency. Online booking systems, automated reminders, and upfront pricing estimates reduce these pain points.
Billing transparency is critical. Patients who understand their bills are 60% more likely to return, according to CareCredit’s healthcare retention study. Offer online payment options, upfront cost estimates, and itemized summaries that demystify charges.
Waiting time reduction also builds loyalty. Even small improvements—like sending real-time text updates for delays—show respect for patients’ time. Friendly front-desk interactions and clean, well-lit waiting areas further reinforce comfort and care.
Finally, review your process quarterly. Analyze complaints or feedback trends, then refine policies accordingly. Friction reduction is not one project—it’s a continuous optimization process.
Track Metrics and Adapt Through Feedback Loops
Retention success starts with data. Key metrics include appointment adherence, average time between visits, referral conversions, and churn rate. Regularly tracking these indicators helps you identify where patients drop off and why.
Visualizing these trends through dashboards can highlight which neurological conditions experience the most attrition. For instance, epilepsy patients may return more consistently than those with migraines, guiding your communication priorities.
Feedback loops are equally powerful. When you respond to patient suggestions, you demonstrate that improvement is ongoing. Clarify Health reports that 76% of patients stay longer with providers who visibly act on feedback.
Continuous adaptation keeps your retention program relevant. Analyze quarterly data, share it with your team, and brainstorm updates to improve care delivery. Retention thrives when insight leads to iteration.

Source: clarifyhealth.com, 2024
Retention Insights for Neurology Practice Growth
Neurology practices that embed retention as a core pillar gain measurable advantages: steadier revenue, stronger relationships, and better outcomes. Each strategy—structured pathways, hybrid care, personalized communication, operational efficiency, and data-driven adaptation—plays a critical role.
When implemented consistently, these approaches create predictable patient experiences and higher trust. Retention becomes more than follow-up scheduling—it becomes a culture of continuity.
To begin improving retention, focus on quick wins such as automating reminders and collecting feedback. Then, scale toward advanced analytics and multi-channel engagement tools.





